- Home
- TREATMENT
- Cleft Lip and Palate
- Corrective Jaw Surgery
- Facial Asymmetry
- Underbite Surgery
- Genioplasty
- V shape Jawline Surgery
- Cyst and Tumour of Jaw
- Wisdom Tooth Surgery
- TMJ Disorders (TMD)
- Rhinoplasty
- Dental Implants
- Ear Reconstruction
- Obstructive Sleep Apnea
- Buccal Fat Pad Removal
- Face & Jaw Bone Fracture
- Minor Oral Surgery
- Facial Aesthetic Surgery
- Double Chin Reduction
- Dental Treatments
- Gallery
- Cleft Lip- Palate Surgery
- Orthognathic Surgery
- Cyst & Tumour of Jaw/Face
- Unilateral Cleft Lip
- Bilateral Cleft Lip
- Why Cleft Lip occurs ?
- Complication in Cleft ?
- What is Cleft Palate ?
- Speech Result
- Youtube Videos
- Jaw Surgery Cost In India
- SURGERY VIDEOS
- Lab Test in Cleft Patient
- Cleft Lip-Dr Parit Ladani
- What Is Cleft Palate ?
- Cleft Lip Repair Surgery
- Alveolar Bone Grafting
- Symmetrical Nose
- Contact Us
- BLOG
Facial Asymmetry Surgery

Why Is My Face Asymmetrical (Crooked Face)?
- Many human body parts undergo development with bilateral symmetry. This implies that the right and left sides can be divided into identical mirror images. However, due to biological factors inherent to processes of development as well as environmental disturbances, perfect bilateral symmetry is rarely found.
- Facial asymmetry is an alteration that is defined by the presence of a disharmony between both sides of the face. That is, in the frontal vertical plane of the face, one of the two sides is unbalanced with respect to the other.
- The face often presents with a mild degree of asymmetry. Nevertheless, slight asymmetry, also known as relative symmetry, subclinical asymmetry or normal asymmetry, ends up being unperceived by its carriers and everyone around them. The prevalence of facial asymmetry is higher than 50% on radiographic examination.
- However, more pronounced asymmetry may become bothersome and in severe cases, are indicative of an underlying syndrome. Facial asymmetry can result from congenital problems, trauma, or a prior surgery or treatment.
- In some cases, asymmetry may affect not only the form, but also the function of your eyes, nose, and mouth. Often, the lower jaw is uneven with the rest of the face. Other problems may include cheek retrusion (backward displacement), eye displacement, eyebrow lowering, forehead and brow bone protrusion, or retrusions and nasal deviations.

Is Facial Asymmetry Normal?
- Yes, it’s perfectly normal for one side of your face to be slightly different or asymmetrical from the other side. Nothing in nature is perfectly symmetric.
- In a symmetrical face, the left and right sides look like each other. They are not perfect mirror images. All faces have some degree of asymmetry which may provide a uniqueness to the face. Natural asymmetry is unlikely to be a cause for concern.
- However, whenever the degree of asymmetry is more severe, the condition is typically rendered noticeable, which negatively affects one's facial and smile aesthetics and interfere with normal functions such as chewing, speaking and breathing. Severe facial asymmetry needs correction for functional and aesthetic reasons.
Is Asymmetrical Face Attractive?
- Facial attractiveness is an important factor in our social interactions. It is still not entirely clear which factors influence the attractiveness of a face and facial asymmetry appears to play a certain role.
- No face is truly symmetrical! There will always be differences between each side of face. Some people's differences are minute, some are more pronounced. In fact, some research indicates that natural asymmetry is both normal and desirable. One of the features that could influence facial attractiveness is mild or sub-clinical facial asymmetry.
- Many study suggest that even in people with pleasing aesthetic profile, there could be subclinical asymmetry which may go unnoticed often as it does not affect the social life of the individual.

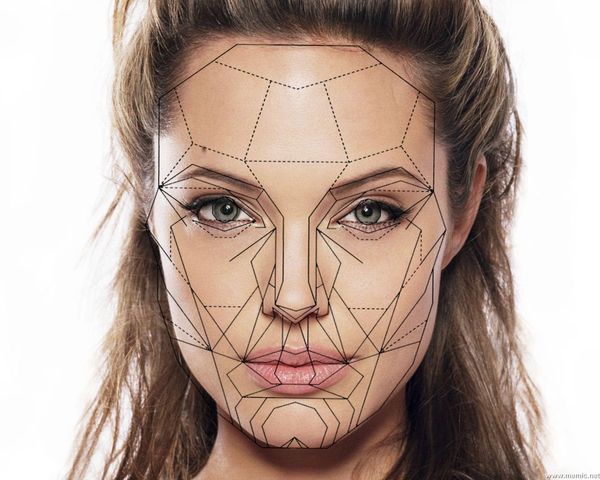
Asymmetrical Face Celebrities
- Even celebrities who we consider to be beautiful would look radically different if their faces were perfectly symmetrical. Everybody has asymmetry in their face and that's perfectly OK.
- It's important to know that nobody actually has a perfectly symmetrical face and mild or subclinical asymmetry is an asset to your beauty. You can see some examples of celebrity in Pictures.

Why is a symmetrical face important?
- It has long been assumed that a symmetrical face is a sign of beauty, compared with an asymmetrical face. Of course, this is a matter of preference and taste, with many finding an asymmetrical face more appealing.
- Minor asymmetries are very common, and nearly everyone is asymmetric to some degree. Even the most state-of-the-art cosmetic procedures can’t accomplish that. The most you can hope to achieve through a surgical or non-surgical facial plastic surgery procedure is to improve the overall alignment of your face and make it look more even than it was before.
- Some people however, have major differences between the two sides of their face, and would like them corrected. The aesthetic and functional problems associated with significant facial asymmetry can very negatively affect the orofacial, nutritional and psychosocial development of the patient.
- Whether you want to improve the minor asymmetries, or to correct the more major structural asymmetry, there are a number of surgical options available to you.

WHAT CAUSES FACIAL ASYMMETRY?
- Number of factors have been highlighted in the development of facial asymmetries. Facial asymmetries could have pathological, traumatic, functional or developmental causal factors.
- The causes of facial asymmetry can be grouped into three main categories:
- Congenital - prenatal origin
- Acquired - resulting from injury or disease
- Developmental - arising during development and of unknown etiology. In many cases, the etiology of facial asymmetry remains unknown and, for this reason, it is termed asymmetry of development. Such idiopathic asymmetries are common in the overall population, but are not found at an early age, appearing gradually throughout craniofacial development.
- Others factors responsible for Facial Asymmetry are :
- Habitual mastication on one side
- Constant facial pressure during sleep exclusively on one side
- Deleterious oral habits or unilateral crossbite
The aforementioned factors would be responsible for increasing unilateral skeletal development.
TYPES OF FACIAL ASYMMETRY AND DIAGNOSIS

TYPES OF FACIAL ASYMMETRY.
Lack of proportion
Extensive research has found that there is a certain optimal ratio of the distance between the main features on the face that makes a person’s face look attractive. According this optimal ratio, also known as the “golden ratio”, the ideal face is around one-and-a-half times as long as it is wide.
The three key facial measurements that are required for determining how close a person’s face is to meeting the “golden” proportions are as follows: Face divide in 3 parts from forehead to chin
Deviation of the lower face is more frequent and greater in length than that of the upper and midface. Deviation of the chin being the most remarkable feature of asymmetry. A possible explanation would be the longer lower jaw (mandibular) growth periods, in addition to the upper jaw (maxilla) being rigidly attached to the stable region of the cranial base.
Because of their developmental origin Aesthetic Facial Asymmetries occur in patterns which can be divided into complete and incomplete types.
Incomplete facial asymmetries are where just one facial feature is affected. The single most common incomplete facial asymmetry is that of the lower jaw. The upper two-thirds of the face are symmetric but the lower jaw is asymmetric.
Complete facial asymmetries are when the entire side of the face is involved and they typically present in two types, a top to bottom pattern (superior facial asymmetry) or a bottom to top pattern. (inferior facial asymmetry). In both types the most affected facial features are either at the top or the bottom of the face and their degree of involvement fades in severity as one moves away from the more severely affected area.
In the superior facial asymmetry, the eyes are seen as the major asymmetric feature. The eyes are at two different levels as judged by a horizontal line drawn through the pupils. Almost always the affected side is the lower eye. But close inspection of the facial features below it can show a downturned mouth corner/lip deviation, nostril asymmetry or even the entire nose pulled toward that side and lower, a fuller jowl on that side as well as chin/jaw lengthening on the asymmetric side.
In the inferior facial asymmetry the lower face is the most serenely affected by chin/jaw deviation or decreased fullness from the other side. The occlusal plane may be level (often because of orthodontic treatment) or even slightly tilted upward on the asymmetric facial side. Similarly the nose will show a nostril that is asymmetric but higher with some slight deviation of the nose.
So while facial asymmetries can involve a wide variety of feature differences between the two sides of the fade (chin/jawline deviation, vertical facial shortening, cheek retrusion, orbital floor/eye displacement, eyebrow lowering, forehead and brow bone protrusion or retrusions and nasal deviations) they generally follow patterns that can be explained by their embryologic development
What involves in Diagnosis of Facial Asymmetry?
Facial Asymmetry is usually caused by the combination of differences in facial length, underlying soft tissues (muscles, fat) and skeletal shape, muscular size and activity, as well as underlying structures. Facial asymmetry must be assessed by thorough and judicious analysis conducted by means of a first interview, extra- and intraoral clinical examination, as well as supplementary diagnostic examination such as radiographs, 3D CT Scan and MRI.
These assessments are necessary to determine what exact procedure(s) would be beneficial and which ones would have the greatest impact on improving facial symmetry. A list of all structures contributing to the asymmetry is made and ordered in priority of importance to the patient. Then the appropriate procedures are matched to the diagnosis list.
The patient then gets to choose which procedures they value and feel will make the greatest amount of improvement. In some cases, all selected procedures may be done at once and in other cases the patient may choose to do only a few or do a staged approach awaiting the outcome of the most important procedures first.
Who are the best candidates for facial asymmetry correction treatment?
- Although a mild non-pathological facial asymmetry is in many cases imperceptible and is often considered normal, its clinical importance cannot be easily determined, since facial aesthetics are completely subjective. Therefore, the degree of acceptance of this malformation will depend largely on the region of asymmetry and the perception of the patient's imbalance.
- That is why not all patients who have facial asymmetry are candidates for surgery, but only those who have a degree of facial asymmetry evident for their social, professional and family environment or that disturbs their peace of mind.
- An asymmetrical face is considered to be unique, charming and attractive. But decision to correct facial deformity is your own. Do you love your asymmetrical face? If not, then you are a candidate for facial asymmetry correction treatment.
Following are some of the reasons for facial asymmetry correction treatment
- People for whom the center line dividing the upper and lower lip is non-straight.
- People who have a non-straight line between the center of the nose and middle of the lips.
- People who have two different chin or jaw lines (left & right).
Correcting facial asymmetry can have many benefits, such as:
- Enhanced aesthetic appearance
- Greater self-confidence
- More youthful appearance
- Better facial function
Whatever the extent of your facial asymmetry, you should ALWAYS consult with a trusted, board-certified Maxillo-Facial Surgeon before making any treatment decisions. Such a professional can evaluate the extent of your facial asymmetry and recommend treatment options that suit your specific needs.
The solution of facial asymmetry, like all surgical procedures that we perform at the Nuface Clinic, solves at the same time aesthetic problems, such as lack of harmony in the factions, and functional, such as pain in the temporomandibular joint or discomfort when chewing , in addition to greatly improving patient self-confidence.
HOW CAN I IMPROVE MY FACE ASYMMETRY?
There are a number of surgical and non-surgical options when it comes to correcting facial asymmetry. The type of procedure you go with typically depends on what your surgeon recommends based on your specific desires and situation.
HOW TO FIX ASYMMETRICAL FACE WITHOUT SURGERY?

Non Surgical Treatment for Facial Asymmetry
- Of course, surgery isn’t necessarily the right choice for everyone and it’s also not the only solution.
- Whether you simply don’t like the idea of going under the knife or you have a medical condition that prevents you from being able to do so, there are alternative non-surgical treatments available to you.
- Slight asymmetries can be effectively addressed using non-surgical or minimally invasive cosmetic treatments. These include:

Facial Injection
- The aim of cosmetic injectables is to improve and restore facial volume, while simultaneously enhancing facial contours and improving any facial asymmetries you may have.
- Dermal Fillers - Tissue fillers can be administered to add volume to one side of a patient’s face, and restore a good balance to your features.
- Botox is used to reduce the prominence of a patient’s jaw or raise an eyebrow that is sitting too low. In some cases, this injectable can even be used to address nasal asymmetries.
- Botox and Filler are used to correct mild facial asymmetries such as:
- One brow is lower than the other.
- One cheek is fuller than the other.
- The smile is crooked and one side of the mouth lifts more than the other.
- Botox and Fillers are popular non-surgical treatment options that a lot of patients choose over surgery because they’re simple, affordable, and can be performed in brief 15 to 20-minute sessions. Not only do Botox and Dermal Fillers plump up your face to make it look more voluminous, youthful, and radiant, but they’re also temporary solutions which means you have more freedom to decide whether you want to continue with a certain look or change it up.

Make up and cosmetics
- If facial asymmetry is very minimal or for some reasons, definite treatment is not possible than Make up and cosmetics can be used.
- There are a variety of cosmetic products, styles, procedures, and strategies you can use to bring balance to your facial features.

Facial Asymmetry And Orthodontics
- Facial asymmetry can be detected in early ages in syndromic cases or during growth of facial bones. One side of facial bones may be slowly growing in comparison to other side of face in such cases. Depending on patient's age and the severity of the condition, a variety of orthodontic and orthopedic treatment options are available with a view to correcting facial asymmetries. This may include myofunctional appliances, asymmetrical extractions or growth modification devices.
- In cases of severe facial asymmetry the treatment of choice should be a combination of Orthodontics and orthognathic surgery. Depending on the degree of dental, skeletal or soft tissue asymmetry, orthodontic treatment or surgical movement must be carried out asymmetrically, so as to achieve symmetry by the end of the therapy.

Facial Asymmetry Correction With Exercises
- A lot of amateur blogs will tell you that facial exercises are a cheap and effective way to treat facial asymmetry. It’s usually not, though. In fact, there are no clinical trials or research that can back up that claim whatsoever.
- In theory, facial exercises would help muscle weakness or uneven muscle tone. The thought process is that, by strengthening the facial muscles, that would appear fuller and more defined. While this is true to an extent, the results are not drastic. Facial asymmetry will continue to pose a problem.
CAN DOCTOR MAKE MY FACE MORE SYMMETRICAL?
Surgical treatment for Facial Asymmetry Correction
- Your doctor will make a thorough examination of your face, using photos and imaging for diagnosis and treatment planning. Together, you’ll discuss in detail your doctor’s recommendations and suggested treatment process.
- Asymmetry can be progressive in nature, while those acquired due to trauma or ablative surgeries are non- progressive. It is prudent for the clinician to consider the aetiology of the asymmetry, the extent and its severity in all three dimensions in order to provide an optimal treatment plan. Besides, it is important to take into consideration factors such as growth, timing of treatment and psychological aspirations of the patients when deciding the treatment plan.
- Any abnormality of the soft or hard tissues of the face can lead to asymmetry. Depending on the issues to be corrected, multiple surgeries may be needed to achieve the desired results. Correction may require moving bone (osteotomy), adding bone (bone graft), adding a facial implant (alloplastic implant), reducing bone, adding soft tissue, or reducing soft tissue (through liposuction) to create a more symmetrical result.
- Because of the myriad of tools that can be used, it’s important that you see a surgeon who is skilled with all techniques so that your treatment isn’t limited by a particular set of tools or approaches. In many cases, your surgeon will work with other specialists to carefully plan treatment both before and after surgery.
- All facial asymmetry surgery procedures are performed under general anesthesia, and certain patients will require an overnight stay in the facility, depending on the number of facial procedures performed and whether they are traveling alone or with someone.
- Facial asymmetry surgery consists of well-known operations that are used for different types of aesthetic and reconstructive facial problems. These include:

Facial Bone Contouring Procedure

Orthognathic Surgery (Jaw Correction Surgery)
- Orthognathic Surgery is the most common type of surgery which can correct asymmetry of the facial skeleton and align the jaws.
- The surgery can be performed on both the upper and lower jaws, and can balance the relationship between the teeth and the improve the symmetry of the face as a whole. Upper jaw surgery is often needed to correct the canting while the lower jaw surgery is needed to achieve a proper bite against the upper as well as to correct the chin point back to the centre.
- Sometimes, after shifting the jaws into the correct position, contouring surgery may be need to reduce the enlarged side.
- Orthognathic surgery, in conjunction with orthodontic treatment, will not only improve the facial harmony and balance but also address the fit and function of the teeth.
Chin Surgery (Genioplasty)
Chin surgery is a procedure to improve the appearance of the chin, and there are a number of different options for this. The chin can be moved forwards or backwards if needed, a procedure known as genioplasty. The size of the chin can also be reduced if needed, and you can also have chin implants to increase the definition of the chin if required.

Cheek Bone Reduction
In cheekbones that are asymmetric by having excessive width, cheekbone reduction osteotomies can be performed. Depending upon the degree and extent back along the zygomatic arch of the excessive width, either an isolated intraoral zygomatic body osteotomy can be done or it may need to be combined with a posterior zygomatic arch osteotomy as well.

Mandibular Angle Reduction
Reduction angleplasty or mandibular angle reduction surgery is a cosmetic surgical procedure done to transform a square shaped face to a more delicate and feminine facial appearance. This surgical procedure is effective in correcting prominent body and angle of the lower jaw, thus reducing the width of lower face and changing a square face to an oval or “V” shaped face. In some cases, mandible angle reduction surgery is combined with other facial contouring surgeries such as zygoma reduction, masseter muscle reduction or genioplasty to correct facial asymmetry. Mandible angle reduction surgery is often performed through intraoral approach hence there is no visible scar externally.

Brow Bone Reduction
The type of brow bone reduction needed in the vertical orbital dystopia type of facial asymmetry is to raise up the lower edge of the brow bone that is too low. The inferior border of the brow bone is removed through an upper eyelid incision (transpalpebral ) by burring to even out the horizontal levels of the bony brow bones.

Facial Implants
- If a person has an asymmetric face due to their skeletal structure, facial implants may be an option to consider. Surgeons use implants to give the appearance of balance in a face.
- According to the association of Oral and Maxillofacial Surgeon of India, surgeons carry out this procedure to enhance the cheeks, chin, and jaw.
Facial implants are meant to be permanent and usually contain:
- Silicone
- Medpore
- Titanium
- PEEK
Various location for Facial Implants.

Cheek Implants (Cheek Bone Augmentation)
- The cheek bones, also known as the zygoma. This zygomatic arch contributes to the broadness of the face when viewed from the front. A more pronounced arch on one side will result in significant asymmetrical appearance. The body of the zygoma, on the other hand, contributes to the frontal projection of the midface.
Most cheek asymmetries are best treated by a custom implant design.
- Restore volume to flat cheeks
- Enhance cheekbone definition
- Add youthful fullness and lifted definition to cheeks

Jaw Implants (Mandibular Angle Implants)
- Expand the lower part of the face to balance out any asymmetry
- Correct a weak jaw, creating a clear delineation between the neck and face
- Create a strong, masculine jawline, which is especially beneficial to male patients

Chin Implant
- Expand the lower part of the face to balance out any asymmetry
- Correct a weak jaw, creating a clear delineation between the neck and face
- Create a strong, masculine jawline, which is especially beneficial to male patients

Orbital Floor Augmentation
The lower asymmetric eyeball can be safely raised to some degree (up to 5mms) by building up the floor of the eye in vertical orbital dystopia. This can be done by a variety of methods from bone grafts to synthetic materials. Because the cheekbone is often affected as well and there is a need to match the orbital floors as closely as possible, a custom designed orbital floor-rim-cheek implant offers the best chance to do so. Placed through a lower eyelid incision the connected inferior orbital bone and cheek can be treated with a single implant.
Soft Tissue Surgery for Facial Asymmetry Correction

Masseter Muscle Reduction
The essential role of masseter muscle is for adequate mastication. Masseter hypertrophy is recognized as an asymptomatic enlargement of one or both masseter muscles. A hypertrophied masseter will alter facial lines, generating discomfort, and create negative cosmetic impacts in many patients. This leads to the prominent mandibular angle which is considered to be aesthetically unacceptable. The muscle function may also be impaired, thus resulting in conditions such as trismus, protrusion, and bruxism. In most cases of masseter hypertrophy, it is bilateral and symmetric, but asymmetry is not unusual.
There are various treatment modalities for the management of masseteric hypertrophy.
TREATMENT MODALITIES
1. Non Surgical Treatment
Injection of botulinum toxin type A (Botox) into the masseter muscle is considered as less invasive modality for the treatment of muscle hypertrophy. Local injection of very small doses of the Botox into a muscle produces local paralysis and therefore, individual muscles can be selectively weakened and atrophy of the muscle occurs. Perhaps the biggest disadvantage of botulinum toxin therapy is that the treatment effect wears away and reverts to the original condition in 4 – 6 months. Unlike surgical excision of muscle tissue that reduces the actual number of muscle cells, botulinum toxin type A only reduces muscle volume temporarily.
2. Surgical Treatment
This surgical treatment consists of removal of 3/4 to 2/3 of all muscle mass via intraoral approach. Occasionally, mandibular cortical bone or angle osteotomy can also be performed at the same time to achieve a streamlined jawline contour. The surgery to access the masseter muscles and the mandible (jawbone) is performed through incisions on the inside of the mouth, between the gum and cheek (lower buccal sulcus area), leaving no visible scarring. Once the correct amount of bone and muscle has been removed, the incision is closed with self-dissolving sutures. The result of surgical approach to masseteric hypertrophy is predictable and longer lasting compared to non surgical method.
Rhinoplasty
Rhinoplasty, which is colloquially known as a nose job, corrects any structural and aesthetic imperfections your nose may have. Straightening a deviated nose usually requires a septorhinoplasty to ensure the central support of the nose gets properly aligned. Nasal osteotomies and tip grafting/alignment are also needed. The nostril on the affected side may be higher to wider which can be aligned by a nostril repositioning procedure. From a crooked nose to a deviated septum, or even if you simply don’t like the shape and size of your nose, rhinoplasty is the solution to contouring and creating perfect symmetry in the central appendage of your face.

Forehead and Brow Lift
Sometimes you can have an uneven number of wrinkles or blemishes on either side of your face or your eyebrows might not be exactly the same shape. A forehead and brow lift can help create facial symmetry by smoothing out any worry lines you may have developed over time and reconfiguring the shape of your brows to make them more uniform so that they suit your face better. A low and asymmetric eyebrow can be treated by several types of browlift techniques.

Facelift/Necklift
Face and neck lifts can do so much more than just even out your skin tone. They can also remove excess fat cells and allow your surgeon to contour your different facial features and eliminate the look of tired eyes and sagging skin. Getting regular face lifts will also help keep your face looking younger by removing dead skin cells to unveil the newer and more vibrant skin underneath.

Buccal Fat Pad removal
Buccal fat pad removal, also known as cheek fat removal or buccal lipectomy, is a surgery that removes excess fat pads from the cheeks to create a more contoured facial appearance. It is generally used to reduce chubby cheeks (“chipmunk cheeks”) that can be due to genetics or weight gain. Buccal fat pad removal is sometimes part of treatment for facial asymmetry correction.

Otoplasty
Commonly referred to as ear surgery, an otoplasty is used to correct issues with large, protruding, or misshapen ears. This procedure can address ears that are too large, deformed, have torn or damaged ear cartilage, or need to be realigned. The procedure can also enhance facial symmetry by reshaping the ears while they are being re-positioned.
For more information.

Corner of Mouth Lift
Downturned corners of the mouth can be lifted and levelled by a pennant skin excision technique with orbicularis wedge muscle excision. In lip asymmetries where the lower position extends beyond just the mouth corner, the length of the pennant can be carried further up along the vermilion-skin edge for a more complete upper lip lifting effect.

Dimple creation
Dimple surgery (also known as dimple creation surgery or dimpleplasty) is an elective plastic surgery procedure that's done to create dimples on the face. Dimples are the small depressions in the cheeks that appear when some people smile. An inherited trait, dimples arise due to indentations in the layer just beneath the skin (called the dermis).
The procedure is typically done on an outpatient basis. The surgery involves the formation of a dimple with the creation of scar tissue in the dermis between the muscles of the face using small instruments and incisions, and a small amount of tissue is removed.1

Upper Eyelid (Ptosis) Repair
In some cases the upper eyelid asymmetry may be due to excessive skin in which an upper blepharoplasty will be corrective. Or the upper eyelid may be hanging lower than the other side relative to its position on the iris of the eye in which an upper eyelid ptosis repair would be needed. But when the eye is being raised in vertical orbital dystopia repair by orbital floor augmentation, it will become more ‘buried’ under the existing position of the upper eyelid in which a ptosis repair will definitely be needed.

Eyelid Canthoplasties/Canthopexies
The lower asymmetric eyeball can be safely raised to some degree (up to 5mms) by building up the floor of the eye in vertical orbital dystopia. This can be done by a variety of methods from bone grafts to synthetic materials. Because the cheekbone is often affected as well and there is a need to match the orbital floors as closely as possible, a custom designed orbital floor-rim-cheek implant offers the best chance to do so. Placed through a lower eyelid incision the connected inferior orbital bone and cheek can be treated with a single implant.
Various Condition Lead to Facial Asymmetry.
Condylar Hyperplasia

Condylar Hyperplasia
Condylar hyperplasia, which is also known as mandibular hyperplasia, is over-enlargement of the mandible bone in the skull. The mandibular bone has two condyles. The condyles are known as the growth centers of the mandible. When the growth in the condyle exceeds its normal time span, it is called condylar hyperplasia. The most prevalent form of condylar hyperplasia is unilateral condylar hyperplasia. In this case, one condyle grows beyond the other condyle which results in facial asymmetry. There are two different categories of condylar hyperplasia, which includes hemimandibular hyperplasia and hemimandibular elongation. An estimated 30% of people who have facial asymmetry have condylar hyperplasia. These two anomalies can be clinically present in a singular form or in combination with one another.
Classification
Type 1- Hemimandibular elongation
- Chin deviation towards contralateral side
- Midline shift towards contralateral side
- Posterior crossbite on contralateral side
- Excessive growth in the horizontal vector
- Enlarged ramus, normal condyle
Type 2 - Hemimandibular hyperplasia
- Sloping rima oris with minimal chin deviation
- Supra-eruption of maxillary molars on affected side
- Open bite
- Midline shift (minimal to none)
- Excessive growth in the vertical vector
- Excessive growth in the condylar head
Type 3 - Combination of both
- Chin deviation towards contralateral side
- Possible open bite
- Sloping rima oris with possible chin deviation
- Combination of excessive growth in both vectors
Cause
Condylar hyperplasia has an unknown cause. One theory states that an event of a trauma leading to increase in number of repair mechanism and hormones in that area may lead to increase in growth of mandible on that side. Another theory states that an increase in loading of the temporomandibular joint can lead to increase in expression of bone forming molecules. Condylar hyperplasia predominantly affects women with 64% of patients being women.
Diagnosis
The diagnosis of asymmetry can be completed through a variety of different methods. PA cephalometry, panoramic radiograph and nuclear imaging are a few of the techniques which can be used for a diagnosis. Primarily nuclear imaging techniques like single-photon emission computed tomography (SPECT), positron emission tomography (PET) and bone scintigraphy are collected along with other data prior to diagnosing a patient with Condylar Hyperplasia. In SPECT imaging, an increase uptake of the isotope is found on the affected side when compared to the non-affected side indicated active growth of condyle on that side. Treatment plan is decided depending on growing status of condyle.
Treatment
There are numerous treatment options for condylar hyperplasia. In some cases, orthognathic surgery can be performed once the active condylar growth has completed. In some cases mandibular bone reshaping such as lower border reduction and angle reduction, is required along with orthognathic surgery. The goal of this surgery to wait while the condyle is growing and complete surgery once the condyle stops growing. This helps reduce the chances of any worsening of facial asymmetry lessens. One downside to this option, however, requires a person to live with their facial asymmetry features until the age of 18 or 19, which can be challenging.
A procedure called condylectomy can also be completed. Condylectomy involves the removal of part of the growing condyle in order to arrest any active growth. Condylectomy can sometimes be done in conjunction with articular disk repositioning and orthognathic surgery in order to treat patients with mandibular hyperplasia.
TMJ Ankylosis

What is Temporomandibular Joint Ankylosis ?
Temporomandibular Joint ankylosis is the condition where the mandibular condyle fuses with the temporal bone (cranial base), thereby resulting in reduced mouth opening. TMJ ankylosis generally affect the younger or the pediatric age group. Its causes can be ear infection, birth trauma, trauma during infancy or childhood or even congenital. If ankylosis occurs during early age or growth period, it leads to disturbance in growth of facial bones specially lower jaw.
What causes ankylosis?
The most common reason for TMJ Ankylosis is untreated or undetected mandibular condylar fracture. If the mandibular condyle fracture goes undetected or is not treated in a proper manner, it leads to unorganised healing of the fracture fragments and frequently leads to the union of mandibular bone with the temporal bone of the cranium. This union initially is in fibrous form and gradually progresses to a more rigid bony ankylosis. For this reason, it is important to assess every trauma to facial region properly to rule out any condylar fracture. If condylar fracture is diagnosed, it becomes essential to manage it appropriately to prevent complications like TMJ Ankylosis.
What happens in TMJ ankylosis?
Most common symptom of TMJ ankylosis is progressive reduction in mouth opening. This directly relates to decreased dietary intake and poor overall growth of the individual. The earlier the ankylosis sets in, the more pronounced affects it has on the growth of the child. Other than just reduced mouth opening, the child also develops facial asymmetry. It results in flattening of one side of the face, shortened mandible, deviation of midline and also malocclusion. If the ankylosis is bilateral, it leads to severely malformed mandible. In severe cases, these shortened mandible causes decreased airway space thereby causing obstructive sleep apnea or commonly known as snoring. Such deformity is known as bird face appearance.
How do you treat TMJ ankylosis and Facial Asymmetry due to that?
In adults, TMJ ankylosis does not lead to facial asymmetry if occurs after completion of facial growth. If there is no facial asymmetry than the treatment of TMJ ankylosis is release of ankylosis and reconstruction of the joint with various materials available.
But the treatment in children or young adults is more challenging as it generally causes malformation of mandible and facial asymmetry as well. For this reason, the treatment options vary from simple ankylosis release along with facial asymmetry correction. In children, Temporomandibular Joint is reconstructed using Costocondral rib graft to facilitate growth of lower jaw. After completion of facial growth, definite surgery is done to correct facial asymmetry. Many procedure is used in correction of facial asymmetry such as, orthognathic surgery, distraction osteogenesis, genioplasty, facial implants and fat injection.
Masseter Muscle Hypertrophy

WHAT IS THE MASSETER MUSCLE?
The masseter muscle runs through the rear part of the cheek, from the cheekbone down to the lower jaw on each side of the face. The muscle connects the mandible (lower jawbone) to the cheekbone and is known as one of the “muscles of mastication” because it works to raise and close the jaw while chewing.
WHY DOES THE MASSETER MUSCLE SOMETIMES NEED TO BE REDUCED?
The masseter can sometimes become enlarged in people who have a tendency to clench or grind their teeth (bruxism), or who chew gum excessively. This may result in an asymmetry of the face due to unequal enlargement and increased bulk of the muscle, potentially creating an overly-square jawline. Typically women, or those seeking facial feminization, prefer a softer, smoother appearance to the jawline, and therefore seek to reduce the size of the masseter.
Masseter Reduction, or Jaw Reduction, is where the lower muscle of the face termed the masseter muscle is reduced. The benefits of this can be two fold. First of all, patients seeking a softer facial shape can improve facial balance and change the shape of an overly square face
Reduction of the masseter may be performed by either 1) surgical, or 2) non-surgical methods…
1. SURGICAL REDUCTION OF THE MASSETER MUSCLE
Surgery to access the masseter and the mandible (jawbone) is performed through incisions on the inside of the mouth, between the gum and cheek, leaving no visible scarring. Your surgeon then shapes and reduces the bone and masseter muscle to achieve a well-rounded, smoother and more streamlined jawline contour. Once the correct amount of bone and muscle has been removed, the incision is closed with self-dissolving sutures.
2. NON-SURGICAL REDUCTION OF THE MASSETER USING BOTOX
Injectable muscle relaxing agents such as Botox work extremely well to non-surgically reduce the masseter muscle and also decrease habitual jaw clenching or teeth grinding (Bruxism). The procedure involves a series of injections of Botox directly into the masseter muscle in small doses over several sessions until the desired appearance is achieved. Depending on the individual, the decreased size of the masseter may stay intact permanently even without further injections.
A common concern with treatment of these muscles with muscle relaxants is that the muscle will freeze and you won’t be able to chew your food. Given the large size of the muscle and the use of other smaller muscles of mastication, chewing is not affected by this treatment, although some people may report feeling a bit ‘funny’ chewing tough foods like steak immediately following treatment.
Hemifacial Microsomia

What is hemifacial microsomia?
Hemifacial microsomia is a congenital condition in which the tissues on one side of the face are underdeveloped. It primarily affects the ear, mouth and jaw areas, though it may also involve the eye, cheek, neck and other parts of the skull, as well as nerves and soft tissue. In 10 to 15 percent of cases, both sides of the face are affected, often times asymmetrically.
Hemifacial microsomia is the second most common facial birth defect behind cleft lip and palate, affecting one in every 3,500 to 4,000 births. The condition is typically nonprogressive, meaning that the areas of the face that are affected at birth will typically remain similarly affected throughout growth and development, neither worsening nor getting better.
Hemifacial microsomia has many names, including: craniofacial microsomia, first and second branchial arch anomaly, branchial arch syndrome, facioauriculovertebral syndrome, oculoauriculovertebral spectrum, and lateral facial dysplasia. Hemifacial microsomia is sometimes confused with Goldenhar syndrome, a rare congenital condition. In fact, hemifacial microsomia is just one of the distinctive characteristics of Goldenhar syndrome, which also includes spine anomalies and epibulbar dermoids or lipodermoids.
What Causes Hemifacial Microsomia?
It is unclear what causes hemifacial microsomia. Research has shown the process starts in the first trimester of pregnancy and may be caused by a vascular problem leading to poor blood supply to the fetus’ face during early development. The facial anomalies are not triggered by a mother’s action or diet.
In the majority of cases, the condition is not inherited, and happens by chance. In a small minority of cases, a child may inherit the condition from his parents. An adult with hemifacial microsomia has about a 3 percent chance or less of having a child with the same condition.
What problems occurs in Hemifacial Microsomia?
Symptoms of hemifacial microsomia range from severe to barely noticeable and depend greatly on the degree of deformity and how much of the face is involved. A child with a mild form of hemifacial microsomia may have a slightly smaller jaw and a skin tag in front of a normal-looking ear. In more severe forms, a child’s face may appear much smaller on one side of his face, with an abnormally shaped or absent ear. (Anotia or Microtia)
People with hemifacial microsomia may have various signs and symptoms, including:
- Facial asymmetry
- Abnormalities of the outer ear such as absence, reduced size (hypoplasia), and/or displacement
- Small and/or flattened maxillary, temporal, and malar bones
- Deafness due to middle ear abnormalities
- Ear tags
- Abnormalities (in shape or number) of the teeth, or significant delay of tooth development
- Narrowed mandible (jaw) or absence of half of the mandible
- Cleft lip and/or palate
- Reduced size of facial muscles
- Abnormalities of the eyes (extremely small or absent)
- Skeletal abnormalities including problems of the spine or ribs
- Absence of cheek muscles or nerves supplying those muscles (resulting in an uneven smile)
Most children with hemifacial microsomia have facial anomalies but no other major medical issues. In some cases, babies born with hemifacial microsomia may also have other health problems such as malformed vertebrae, heart defects or abnormally shaped kidneys.
How to diagnose Hemifacial Microsomia?
The diagnosis of hemifacial microsomia can be made before or after birth. Some of the abnormal facial features are visible during prenatal ultrasound. The majority of children are not diagnosed with hemifacial microsomia until after birth. In this case, experts Craniofacial Surgeon will evaluate your child. Experienced Craniofacial Surgeon will make the diagnosis based on your child’s appearance: the mandibular (jaw) deformity is the hallmark of hemifacial microsomia, and is classified based on the development of the jaw. Diagnostic tests such as X-rays and CT scans may also be used to better examine your child’s bone and cartilage structure in order to make appropriate treatment recommendations.
How do they treat Hemifacial Microsomia?
The treatment of hemifacial microsomia varies tremendously from patient to patient and depends on the severity of the condition and long-term needs of the child. Consultation with an experienced craniofacial team is extremely important in achieving the best outcomes for your child.
At Nuface Clinic, we have expertise in every pediatric craniofacial surgery, your child will have access to a multidisciplinary healthcare team and coordinated care through our Craniofacial Team. We will work with you to prioritize your child’s needs and establish a comprehensive treatment plan that addresses both physical and psychosocial needs, including planning for staged surgical repair and reconstruction.
Timing can be a critical factor in treatment of hemifacial microsomia. In some cases, treatment can wait until your child reaches certain developmental milestones.
Supportive treatment at birth
· If your child is born with hemifacial microsomia, he may require respiratory support or a tracheostomy if the jaw is severely deficient. In most cases, your child’s airway can be managed conservatively.
· Due to the presence of the jaw deformity and clefts, your child may experience feeding difficulties. He may receive supplemental feedings through a nasogastric tube to support his growth and weight gain.
· If facial paralysis or eyelid abnormalities are present, eye closure may be incomplete and eye protection must be provided either via lubricants or surgical procedures.
Surgical treatment
As your child with hemifacial microsomia grows, he may need surgical treatment based on the severity and area affected. Not all children with hemifacial microsomia have problems in all of these areas.
Below are some of the interventions your child may need.
Ears
Some children with abnormally-shaped or missing ears may choose to have a series of reconstructive surgeries to make the ear appear more normal. The first surgery typically occurs after age 9, when your child’s ears have almost reached adult-size. Another option is to make an artificial or prosthetic ear, which also requires several surgeries.
For more information on Ear Reconstruction Surgery.
Eyelid differences
For children with eyelid differences, surgical procedures to reposition the lower lids and corners of the eyes may be required.
Soft tissue deficiencies
Children with skin, cheek and other soft tissue deficiencies may need augmentation procedures such as fat grafting or tissue transfer.
Cleft lip/cleft palate
Babies born with cleft lip or palate can have surgical repairs done during the child’s first year. Cleft lip repair is typically performed when your child is 3 to 6 months old, while cleft palate surgery is generally performed when your child is about a year old.
Lateral facial cleft
A lateral facial cleft is one of the most severe deficiencies found with hemifacial microsomia. It requires a staged reconstruction, similar to the process used in routine repair of cleft lip and palate. In this procedure, surgeons will create a ring of muscle around your child’s mouth, connecting the corners and drawing up the lateral line of the lower lip. This reconstructive procedure also helps with feeding and speaking.
Bony deficiencies
In mild cases of bony deficiencies, no treatment may be needed. In more severe cases, surgery may be required. Two of the most commonly performed procedures include distraction lengthening of the mandible (most common) and reconstruction of the mandible with a rib or free vascularized fibula graft (less common).
For a distraction lengthening of the mandible, a surgeon cuts the mandible (jaw) in the center of its deficient region and implants a small device that allows the two bone segments to be distracted (pulled apart), creating a gap in the bone. New bone begins to form in the gap of the small jaw and the device is slowly widened until the jaw is appropriately-sized. When the jaw bone has been adjusted, it improves facial form and the way the top and bottom teeth fit together. Mandibular distraction may need to be repeated as your child grows.
As is the case for any patient with a complex craniofacial deformity, individual treatment varies depending upon the degree of involvement of the various structures. Your child’s individual treatment plan may vary from others similarly affected due to a variety of other factors. It is important that you see an experienced craniofacial team to manage and assess your child’s condition.
Follow-up care
As your child with hemifacial microsomia grows into adolescence, he should continue to be monitored by experienced physicians who can adjust treatment plans as needed.
Because multiple body systems may be involved in hemifacial microsomia, continued monitoring for complications and any treatment as needed are important to optimal long-term outcomes.
Fibrous dysplasia

What is craniofacial fibrous dysplasia?
Craniofacial fibrous dysplasia is a bone disease of the face and skull that replaces normal bone with fibrous-type tissue. This tissue is not as hard as normal bone, and because it is soft and stringy, it makes the bone more fragile and prone to break. Craniofacial fibrous dysplasia is related to fibrous dysplasia, which can affect any bone in the body but most commonly affects the long bones in the legs and arms. The condition, sometimes called facial fibrous dysplasia or fibrous dysplasia of the skull, may affect one bone or multiple bones. Craniofacial fibrous dysplasia may cause shifting of facial features and facial asymmetry, such as incorrect placement of the eyes, misalignment of the jaw, and other problems.
There are two forms of fibrous dysplasia:
· Monostotic, which affects one bone and is active while the child is growing but often becomes inactive after puberty
· Polyostotic, which affects multiple bones and may remain active throughout a person’s life
Fibrous dysplasia may appear in childhood, usually between the ages of 3 and 15. Boys are more often diagnosed with fibrous dysplasia than girls, except one specific type of polyostotic fibrous dysplasia — McCune-Albright syndrome — which is more common in girls and affects the bones and skin and is associated with hormonal imbalance and often precocious (premature) puberty.
What Causes Cranifacial Fibrous Dysplasia?
While the exact cause of fibrous dysplasia is unknown, recent studies point to a mutation of Gs alpha protein during prenatal development as a contributing factor. Fibrous dysplasia is not hereditary, meaning parents do not pass the condition to their children.
What problems occurs in fibrous dysplasia?
Signs and symptoms of fibrous dysplasia affecting the skull may include:
· Facial asymmetry
· Shifting facial structure that can affect any bone in the face
· Nasal airway obstruction
· Jaw and bite misalignment, in some cases making it difficult to chew and swallow
· Visual and hearing problems due to compression of the optic nerve or acoustic nerve
· Additionally, children with craniofacial fibrous dysplasia may experience symptoms related to bone weakness in other parts of the body, including bone fractures or deformities, bone pain, or bone lesions which may stop growing when the child reaches puberty.
Children with polyostotic fibrous dysplasia may also experience:
· Endocrine gland problems, such as early puberty, thyroid disorders and related issues
· Unusual skin patches, called café-au-lait pigmentation, ranging from light brown to dark brown in color
How do they treat Craniofacial Fibrous Dysplasia?
At The Nuface Clinic, your child's diagnostic evaluation begins with a thorough medical history and physical examination. Clinical experts use a variety of diagnostic tests to diagnose facial fibrous dysplasia such as X-rays and CT Scan with constructed 3D images, which are used for intervention planning.
Depending on your child’s condition and symptoms, clinicians may recommend additional testing including blood work and hormone testing.
Treatment
At Nuface Clinic, experts Craniomaxillofacial Surgeon take a team approach to treatment of fibrous dysplasia of the skull. Specialists from Craniomaxillofacial surgery, neurosurgery and ophthalmology collaborate to provide your child with individualized care and the best possible outcomes.
Surgical treatment
While several surgical options are available to treat facial fibrous dysplasia, your child’s treatment will depend on the location of the bones affected and the severity of the condition.
Surgery is usually done through limited incision approaches and hidden incisions in the hair. This can help reduce visible scarring.
· If the affected areas of the face are small and easily accessible, treatment usually involves complete surgical removal (resection) of the area and reconstruction using a combination of bone grafts and materials such as titanium plates and screws.
· If the area affected is too large or too important to be removed, the size of the bone may be reduced to normal using a high speed burr. The procedure is know as cosmetic shaving of bone. If the facial fibrous dysplasia is in an area where it is growing and compressing nerves, removing some of the surrounding bone can decompress the nerve.
· In some patients, a combination of bone reduction with a burr and bone grafting may be utilized.
· In severe cases where the jaw is displaced and malocclusion occurs, a combined therapy with orthodontics will utilize osteotomies (bone cuts) to reposition abnormally placed bones.
· If surgery is required on a particular facial region such as the skull base, your craniomaxillofacial surgeon may work together with a neurosurgeon or ophthalmologist to ensure the most effective treatment. If your child's condition involves the jaw, craniomaxillofacial surgeons will collaborate with orthodontics if needed.
· Your child may need additional surgeries over the course of treatment for facial fibrous dysplasia. In severe cases, the excess bone may grow back over time and require repeated treatments.
After surgery for facial fibrous dysplasia, your child should expect to stay overnight in the Hospital. Depending on the complexity of the surgery required, your child may be hospitalized anywhere from one to several days.
Follow-up care
Your child will need to return for evaluation approximately one to two weeks after surgery. Regular follow-up visit will be needed and are commonly done every three months for the first year, and then yearly, based on your child's condition.
In cases where the bone has been shaped or contoured — usually to preserve vital structures and because the disease affects a large volume of bone — recurrence of the bony overgrowth may occur and secondary procedures may be necessary.
During follow-up visits, your child’s physician will perform a physical exam and may order X-rays or CT scan of the affected area until your child reaches skeletal maturity. If your child was diagnosed with polyostotic fibrous dysplasia, he may also be referred to an endocrinologist for periodic testing of any endocrine or hormone related disorder.
Outcomes for children treated for craniofacial fibrous dysplasia have been excellent. Because this disease is persistent, continued clinical monitoring is essential in long-term management of the condition.
Progressive Hemifacial Atrophy (Parry Romberg Diseases)

What is Progressive Hemifacial Atrophy (Parry Romberg Diseases)?
Progressive hemifacial atrophy (PHA), also known as Parry-Romberg syndrome, is characterized by slowly progressive deterioration of the skin and soft tissues on one side of the face. It sometimes occurs on both sides of the face and occasionally involves the arm, trunk, and/or leg. The number of people affected by progressive hemifacial atrophy is not well-established, but the prevalence is estimated to be about 1 in 700,000. The condition appears to affect females more frequently than males.
Most cases of progressive hemifacial atrophy are sporadic, which means they occur in people with no family history of the condition. However, in rare cases, more than one family member is affected. No clear pattern of inheritance in these cases has been seen.
The condition may worsen for 2 to 20 years and then stabilize. It usually begins around age 10 but can begin as early as infancy or as late as mid-adulthood. The severity varies greatly. While the cause is not well understood, it may differ among affected people. After progressive hemifacial atrophy has stopped progressing, reconstructive surgery may be used to restore the natural shape of the face and eye.
What Causes Cranifacial Fibrous Dysplasia?
While the exact cause of fibrous dysplasia is unknown, recent studies point to a mutation of Gs alpha protein during prenatal development as a contributing factor. Fibrous dysplasia is not hereditary, meaning parents do not pass the condition to their children.
What problems occurs in fibrous dysplasia?
Signs and symptoms of fibrous dysplasia affecting the skull may include:
· Facial asymmetry
· Shifting facial structure that can affect any bone in the face
· Nasal airway obstruction
· Jaw and bite misalignment, in some cases making it difficult to chew and swallow
· Visual and hearing problems due to compression of the optic nerve or acoustic nerve
· Additionally, children with craniofacial fibrous dysplasia may experience symptoms related to bone weakness in other parts of the body, including bone fractures or deformities, bone pain, or bone lesions which may stop growing when the child reaches puberty.
Children with polyostotic fibrous dysplasia may also experience:
· Endocrine gland problems, such as early puberty, thyroid disorders and related issues
· Unusual skin patches, called café-au-lait pigmentation, ranging from light brown to dark brown in color
How do they treat Craniofacial Fibrous Dysplasia?
At The Nuface Clinic, your child's diagnostic evaluation begins with a thorough medical history and physical examination. Clinical experts use a variety of diagnostic tests to diagnose facial fibrous dysplasia such as X-rays and CT Scan with constructed 3D images, which are used for intervention planning.
Depending on your child’s condition and symptoms, clinicians may recommend additional testing including blood work and hormone testing.
Treatment
At Nuface Clinic, experts Craniomaxillofacial Surgeon take a team approach to treatment of fibrous dysplasia of the skull. Specialists from Craniomaxillofacial surgery, neurosurgery and ophthalmology collaborate to provide your child with individualized care and the best possible outcomes.
Surgical treatment
While several surgical options are available to treat facial fibrous dysplasia, your child’s treatment will depend on the location of the bones affected and the severity of the condition.
Surgery is usually done through limited incision approaches and hidden incisions in the hair. This can help reduce visible scarring.
· If the affected areas of the face are small and easily accessible, treatment usually involves complete surgical removal (resection) of the area and reconstruction using a combination of bone grafts and materials such as titanium plates and screws.
· If the area affected is too large or too important to be removed, the size of the bone may be reduced to normal using a high speed burr. The procedure is know as cosmetic shaving of bone. If the facial fibrous dysplasia is in an area where it is growing and compressing nerves, removing some of the surrounding bone can decompress the nerve.
· In some patients, a combination of bone reduction with a burr and bone grafting may be utilized.
· In severe cases where the jaw is displaced and malocclusion occurs, a combined therapy with orthodontics will utilize osteotomies (bone cuts) to reposition abnormally placed bones.
· If surgery is required on a particular facial region such as the skull base, your craniomaxillofacial surgeon may work together with a neurosurgeon or ophthalmologist to ensure the most effective treatment. If your child's condition involves the jaw, craniomaxillofacial surgeons will collaborate with orthodontics if needed.
· Your child may need additional surgeries over the course of treatment for facial fibrous dysplasia. In severe cases, the excess bone may grow back over time and require repeated treatments.
After surgery for facial fibrous dysplasia, your child should expect to stay overnight in the Hospital. Depending on the complexity of the surgery required, your child may be hospitalized anywhere from one to several days.
Follow-up care
Your child will need to return for evaluation approximately one to two weeks after surgery. Regular follow-up visit will be needed and are commonly done every three months for the first year, and then yearly, based on your child's condition.
In cases where the bone has been shaped or contoured — usually to preserve vital structures and because the disease affects a large volume of bone — recurrence of the bony overgrowth may occur and secondary procedures may be necessary.
During follow-up visits, your child’s physician will perform a physical exam and may order X-rays or CT scan of the affected area until your child reaches skeletal maturity. If your child was diagnosed with polyostotic fibrous dysplasia, he may also be referred to an endocrinologist for periodic testing of any endocrine or hormone related disorder.
Outcomes for children treated for craniofacial fibrous dysplasia have been excellent. Because this disease is persistent, continued clinical monitoring is essential in long-term management of the condition.
What are the risks of facial asymmetry surgery?
What are the risks of facial asymmetry surgery?
As with any surgery, facial surgery does pose some risks. These risks include:
· Anesthesia complications
· Bleeding
· Bruising
· Damage to bone, eyes, ears, nose, teeth, or gums
· Infection
· Nerve damage
· Numbness
· Pain
· Swelling
· Additional surgery may be required to address complications or unanticipated anomalies in healing
HOW LOGN DOES IT TAKE TO TREAT FACIAL ASYMMETRY?
· While facial asymmetry surgery may involve a single procedure, more commonly it includes multiple facial procedures. As a result, the after effects such as facial swelling and bruising vary significantly from patient to patient.
· Depending on how extensive the surgery is, you may return home the same day or spend a night or two in the hospital. You’ll return home with instructions and medications from your doctor.
· Immediately after the operation, your face will feel swollen and tight. It is advised to use ice packs right after the surgery until swelling goes down. Swelling and pain will typically peak a few days after surgery, and then resolve within a few weeks.
· You need to wear a facial compression band for at least 5 days after the surgery and avoid bending your head down or lying on the stomach.
· Having normal food is possible two weeks after the surgery. You should avoid smoking and drinking alcohol for at least one month after the procedure.
· The stitches will be removed after 7-10 days.
· The length of recovery is not based on pain but rather on swelling and the time it takes to look more normal again. It could take anywhere from two to three weeks for one to feel completely comfortable being in public without having noticeable signs of surgery.
· The most important thing to understand is that facial asymmetry surgery is about lessening the degree of asymmetry; perfect facial symmetry is usually not possible. In many patients, it may take more than one surgery to attain the best possible result.
WHICH DOCTOR TO CONSULT FOR FACIAL ASYMMETRY?

WHICH DOCTOR TO CONSULT FOR FACIAL ASYMMETRY?
Facial symmetry surgery is a cosmetic procedure that combines the use of facial fillers with surgical procedures to enhance patients’ facial symmetry. The procedure is unique to each individual as the specific treatments recommended depend on the areas causing asymmetries and the patient’s personal goals and desired look. A consultation with a Board Certified Oral and Maxillofacial Surgeon is essential before undertaking any procedure. They will conduct a thorough assessment of your facial structure and ensure the procedure enhances the overall symmetry of your face. Dr. Parit Ladani is one of the best Oral and Maxillofacial Surgeon in India with extensive experience in correcting complex facial asymmetry cases.
When planning your surgery, our team will thoroughly analyze all the elements that make up the facial area: jaw, maxilla, maxillary buttresses, nose, teeth and all the soft tissue that covers the facial skeleton and neck region to correct the facial asymmetry and find the ideal balance of your features.
It is also important to keep in mind that a large majority of orthognathic surgery patients have some degree of facial asymmetry, which makes Dr. Parit Ladani one of the most experienced in this area in India, with an average of 100 orthognathic surgery operations per year.
HOW MUCH DOES FACIAL ASYMMETRY SURGERY COST IN INDIA?
Facial asymmetry surgery cost needs to be determined individually during a one-on-one consultation with your oral and maxillofacial surgeon. Facial asymmetry is unique to each patient so the number and complexity of the procedures required will differ greatly in each case. Additional cost considerations include the experience of the oral and maxillofacial surgeon and any hospital or facility fees required.
Is facial asymmetry covered by insurance?
Insurance coverage is often available when your insurance carrier determines the procedures to be medically necessary to address deformities or functional problems. It is always best to discuss coverage with your insurance carrier and the steps necessary for approval. Our office will assist you with the paperwork needed for pre-approval.
Frequently Asked Questions
Please reach us at drparitladani@gmail.com if you cannot find an answer to your question.
You may be a good candidate if:
· You’re physically healthy
· Your expectations are realistic
· You understand the risks that come along with surgery
· You’re unhappy with your face’s proportion or balance
· You experience functional impairments because of your face’s asymmetry
Sleeping on a favoured side can weaken the area where the skin naturally folds making them deeper on that side. Poor Posture and resting your face on your hand have been attributed to facial asymmetries. Sun damage & smoking have effects on the elastin, collagen and pigmentation, which can be attributed to asymmetry.
Cost for Jaw surgery depends on its complexity and varies for different Hospital setup. Average cost for Bijaw surgery is approx 150000/-, One Jaw Surgery is 80000/- and Genioplasty is 50000/-.
Nuface Cleft and Maxillofacial Surgery Clinic
B-105/106, Dhanashree Height, Bldg No. 42, Azad Nagar 2, Veera Desai Rd, Andheri W, Mumbai. 400053

