- Home
- TREATMENT
- Cleft Lip and Palate
- Corrective Jaw Surgery
- Facial Asymmetry
- Underbite Surgery
- Genioplasty
- V shape Jawline Surgery
- Cyst and Tumour of Jaw
- Wisdom Tooth Surgery
- TMJ Disorders (TMD)
- Rhinoplasty
- Dental Implants
- Ear Reconstruction
- Obstructive Sleep Apnea
- Buccal Fat Pad Removal
- Face & Jaw Bone Fracture
- Minor Oral Surgery
- Facial Aesthetic Surgery
- Double Chin Reduction
- Dental Treatments
- Gallery
- Cleft Lip- Palate Surgery
- Orthognathic Surgery
- Cyst & Tumour of Jaw/Face
- Unilateral Cleft Lip
- Bilateral Cleft Lip
- Why Cleft Lip occurs ?
- Complication in Cleft ?
- What is Cleft Palate ?
- Speech Result
- Youtube Videos
- Jaw Surgery Cost In India
- SURGERY VIDEOS
- Lab Test in Cleft Patient
- Cleft Lip-Dr Parit Ladani
- What Is Cleft Palate ?
- Cleft Lip Repair Surgery
- Alveolar Bone Grafting
- Symmetrical Nose
- Contact Us
- BLOG
Temporomandibular Joint Disorders (TMD)
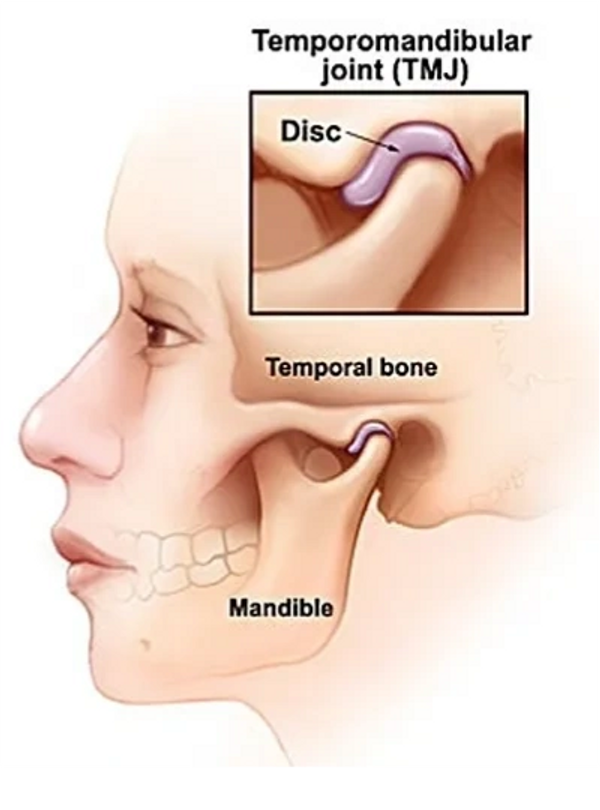
What is Temporomandibular Joint?
- The temporomandibular joint is a hinge-like joint located where your jawbone and skull meet. TMJ is an acronym that stands for temporomandibular joint. The temporomandibular joint combines a hinge action with sliding motions.
- The parts of the bones that interact in the joint are covered with cartilage and are separated by a small shock-absorbing disk, which normally keeps the movement smooth.
- You have one joint on each side of your jaw. The TMJ allows your jaw to slide up and down, letting you talk, chew, and do all sorts of things with your mouth.
What is TMD?
- TMD stands for temporomandibular joint disorder. TMD is the general term used to describe pain and/or dysfunction of the masticatory apparatus including the temporomandibular joint, masticatory muscles, and supporting structures.Many people use the terms TMJ and TMD interchangeably.
- Painful TMJ disorders can occur if:
- The disk erodes or moves out of its proper alignment
- The joint's cartilage is damaged by arthritis
- The joint is damaged by a blow or other impact
- When the muscles and ligaments around your jaw joints become inflamed or irritated.
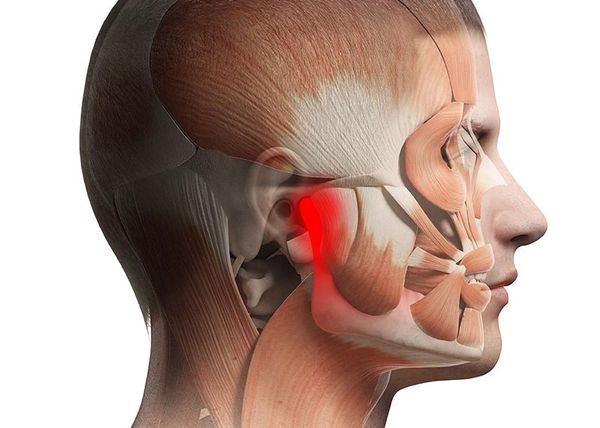
- A TMJ Disorder causes pain, stiffness, or lack of mobility in your TMJ, keeping you from using your jaw’s full range of movement. The condition may be acute or chronic, and the resulting pain may be mild or severe.

What causes temporomandibular joint disorder (TMD) ?
- The exact cause of a person's TMJ disorder is often difficult to determine.Your pain may be due to a combination of factors, such as genetics, arthritis or jaw injury.
- TMJ disorder can be caused by
- Injury to your jaw, the joint, or the muscles of your head and neck -- like from a heavy blow or whiplash.
- Bruxism (teeth grinding/clenching)which puts a lot of pressure on the joint.
- Dislocation of the disc between the ball and socket joint.
- Arthritis in the TMJ.
- Stress, which can cause you to tighten facial and jaw muscles or clench the teeth.
- Acute trauma.
- An improper bite.

What Are the Symptoms of TMD?
Pain and swelling
- Pain or tenderness in your face, jaw joint area, neck and shoulders, and in or around the ear when you chew, speak, or open your mouth wide. Swelling on the side of your face.
- You may also have toothaches, headaches, neck aches, dizziness, earaches, hearing problems, upper shoulder pain, and ringing in the ears (tinnitus).
Lock Jaw
- Problems when you try to open your mouth wide.
- Jaws that get "stuck" or "lock" in the open- or closed-mouth position
Clicking, Popping and Grating Sound
- Clicking, popping, or grating sounds in the jaw joint when you open or close your mouth or chew. This may or may not be painful.
Trouble with Jaw function
- A tired feeling in your face. Trouble chewing or a sudden uncomfortable bite -- as if the upper and lower teeth are not fitting together properly.
Diagnosis and Investigations for TMD

How is TMJ dysfunction diagnosed?
Many other conditions cause similar symptoms -- like tooth decay, Ear ache, sinus problems, arthritis, or gum disease. To figure out what’s causing yours, the Oral and Maxillofacial Surgeon will ask about your health history and conduct a physical exam.
They’ll check your jaw joints for pain or tenderness and listen for clicks, pops, or grating sounds when you move them. They’ll also make sure your jaw works like it should and doesn’t lock when you open or close your mouth. Plus they’ll test your bite and check for problems with your facial muscles.
In addition, radiographs (X-rays) may be taken to view the jaw joints and determine the extent of damage. These may include:
- Panoramic X-rays. This type of dental X-ray shows a broad overview of your teeth, jawbone and TMJs.
- CBCT scans. Cone beam computed tomography (CBCT) scans capture thousands of images of your teeth, jaws, facial bones and sinuses. These pictures are then stitched together for a detailed 3-D image. Dental CT scans give your healthcare provider a more detailed view of your facial anatomy.
- MRI scans. In some cases, magnetic resonance imaging (MRI) may be used to view soft tissues in and around the jaw joints. These images show the position of the disk, inflammation and possible jaw locking. This can tell your healthcare provider if the TMJ disc is functioning properly and in good condition.
- TMJ arthroscopy is sometimes used in the diagnosis of a TMJ disorder. During TMJ arthroscopy, your doctor inserts a small thin tube (cannula) into the joint space, and a small camera (arthroscope) is then inserted to view the area and to help determine a diagnosis.
How to Prepare for your appointment with TMJ Specialist?
You'll probably first talk about your TMJ symptoms with your family doctor or dentist. If suggested treatments don't provide enough relief, you may be referred to a doctor who specializes in TMJ disorders.
What you can do?
You may want to prepare a list that answers the following questions:
· When did your symptoms begin?
· Have you ever had this occur in the past?
· Has your level of stress increased recently?
· Do you have frequent headaches, neck aches or toothaches?
· What medications and supplements do you take regularly?
· What to expect from your TMJ Specialist
Your doctor may ask some of the following questions:
· Is your pain constant or do your symptoms come and go?
· Does any activity seem to trigger the pain?
· Does your jaw click or pop when you move it? Is that clicking painful?
· Is it difficult to open your mouth normally?
Your Surgeon will ask additional questions based on your responses, symptoms and needs. Preparing and anticipating questions will help you make the most of your time.

What are different TMJ Problems?
TMD may be classified as articular (within the joint) or non-articular (outside the joint).
Articular Type
Non Articular Types
Temporomandibular Joint Disorders (TMD)

What is Myofascial pain dysfunction syndrome (MPDS) ?
- Non-articular disorders commonly present as masticatory muscle dysfunction associated with poorly localized pain and a symmetrically reduced range of mandibular motion.
- Synonyms for this condition include Myofascial pain dysfunction (MPD), TMJ dysfunction syndrome, craniomandibular dysfunction and facial arthromyalgia.
- Non-articular TMD is a more common entity than are the articular TMD counterparts. Response to conservative, reversible, non-interventional therapy is usually good. Conversely, surgical intervention is of no value in musculo-ligamentous disorders.

What is Temporomandibular Joint Internal Derangement?
- The term “internal derangement” is used to describe alterations in disc-fossa relations. Internal derangements may be associated with any of the articular etiologies.
- Internal Derangement may present with signs and symptoms quite similar to the more common non-articular TMD.
- As a result, an accurate diagnosis can be more difficult for the inexperienced clinician. However, more localized pre-auricular pain and the likelihood of asymmetric mandibular function such as ipsilateral deviation on opening and restricted lateral excursions to the contralateral side suggest an articular disorder.

What is Temporomandibular Joint Hypermobility?
- Hypermobile Temporomandibular joints are those joints that are prone to frequent and recurrent subluxation or dislocation. In either scenario, hypermobility actually refers to a situation in which the mandibular condyle translates beyond its normal range with respect to the articular eminence.
- The possible etiologies of TMJ hypermobility include: overextension injuries, trauma, connective tissue disorders that result in laxity of the TMJ capsule and ligaments, internal derangement and degenerative joint disease.
- Subluxation refers to an incomplete dislocation of the mandibular condyle, whereby the condyle translates beyond the articular eminence on opening, but either spontaneously returns to or can be manipulated back into the glenoid fossa by the patient.
- Complete dislocation represents the most extreme scenario with respect to a hypermobile TMJ. It occurs when the mandibular condyle moves into a position anterior to the articular eminence resulting in mandibular “open-lock”. In this case, the mandibular condyle cannot be self-reduced and usually requires immediate attention.
- Most severe TMJ hypermobility conditions can effectively be managed by manual reduction followed by a period of complete rest for at least two weeks. After the initial episode, patients are educated about hypermobility and are strongly advised to avoid any potential triggers.
- Surgical management of TMJ hypermobility is reserved for either acute TMJ dislocations that cannot be manually reduced, chronic dislocation where the mandibular condyle has been dislocated for an extended period of time, or a pattern of recurrent dislocation that is occurring with increasing frequency and is adversely effecting one’s quality of life.

What is Temporomandibular Joint Ankylosis?
- TMJ ankylosis usually develops as a result of trauma, inflammation, sepsis, and/or systemic diseases causing severely limited jaw function as well as oral hygiene and nutritional problems.
- When this condition occurs during the growing years, it can severely affect jaw growth and development. In unilateral ankylosis, the other condyle will continue to grow but may be retarded in its true growth potential.
The common clinical and radiographic characteristics of TMJ ankylosis, particularly when occurring in children, include:
- Decreased jaw mobility and function.
- Decreased growth on the involved side.
- Facial asymmetry if unilateral involvement with the mandible shifted towards the ipsilateral side.
- Retruded mandible.
- Usually a Class II occlusion.
- Radiographic and MRI evidence of bony ankylosis between the condyle and the fossa or heterotopic bone surrounding the joint.
The most predictable treatment for the ankylosed TMJ patient includes:
- Release of the ankylosed joint; removal of the heterotopic and reactive bone with thorough debridement of the TMJ and adjacent areas.
- Reconstruct the TMJs (and if indicated, advance the mandible) with a custom-fitted total joint prosthesis.
- Coronoidotomies or coronoidectomies if the ramus is significantly advanced or vertically lengthened with the prosthesis.
- Autogenous fat graft (harvested from the abdomen or buttock) packed around the prosthesis in the TMJ area.
- Additional orthognathic surgery if indicated.
- In these cases it is absolutely necessary that fat grafts be packed around the articulating parts of the prosthesis to prevent the reoccurrence of heterotopic and reactive bone as well as minimize fibrosis.
Other Temporomandibular Joint Pathology

Infectious arthritis
Infection of the temporomandibular joint (TMJ) may result from direct extension of adjacent infection or hematogenous spread of bloodborne organisms. The joint area is inflamed, and jaw movement is limited and painful. Local signs of infection associated with evidence of a systemic disease or with an adjacent infection suggest the diagnosis. X-ray results are negative in the early stages but may show bone destruction later. If suppurative arthritis is suspected, the joint is aspirated to confirm the diagnosis and to identify the causative organism. Diagnosis must be made rapidly to prevent permanent joint damage.
Treatment includes antibiotics, proper hydration, pain control, and motion restriction. Suppurative infections are aspirated or incised and drained. Once the infection is controlled, passive jaw-opening exercises help prevent scarring and limitation of motion.
Traumatic arthritis
Rarely, acute injury may lead to arthritis of the TMJ. Pain, tenderness, and limitation of mandibular motion occur. Diagnosis is based primarily on history. X-ray results are negative except when intra-articular edema or hemorrhage widens the joint space. Treatment includes oral corticosteroids, nonsteroidal anti-inflammatory drugs (NSAIDs), application of heat, a soft diet, and restriction of jaw movement.
Osteoarthritis
The TMJ may be affected by osteoarthritis (degenerative joint disease), usually in people > 50 years. Occasionally, patients complain of stiffness, a grating sound on jaw movement, or mild pain. Crepitus may result from disk degeneration or perforation, causing bone to grate on bone. Joint involvement is generally bilateral. X-rays or cone beam CT may show flattening (eg, subchondral cysts, erosions and lipping of the condyle, suggestive of dysfunctional change, most likely due to excessive loading of the joint). Treatment is symptomatic. An oral appliance (mouth guard) worn during sleep (and possibly while awake) may help alleviate pain and reduce grating sounds.
Secondary degenerative arthritis
This arthritis usually develops in people (usually women) aged 20 to 40 years with a history of trauma or persistent myofascial pain syndrome. It is characterized by limited opening of the mouth, unilateral pain during jaw movement, joint tenderness, and crepitus. When it is associated with myofascial pain syndrome, symptoms wax and wane.
Unilateral joint involvement helps distinguish secondary degenerative arthritis from osteoarthritis. Diagnosis is based on x-rays, which, as in osteoarthritis, generally show condylar flattening, lipping, spurring, or erosion.
Treatment is conservative, as it is for myofascial pain syndrome, although arthroplasty or high condylectomy may be necessary. An oral appliance (occlusal splint [mouth guard]) usually relieves symptoms. The appliance is worn constantly, except during meals, oral hygiene, and appliance cleaning. When symptoms resolve, the length of time that the appliance is worn each day is gradually reduced. Intra-articular injection of corticosteroids may relieve symptoms but may harm the joint if repeated often.
Rheumatoid arthritis
The TMJ is affected in > 17% of adults and children with rheumatoid arthritis, but it is usually among the last joints involved. Pain, swelling, and limited movement are the most common findings. In children, destruction of the condyle results in mandibular growth disturbance and facial deformity. Ankylosis may follow. X-rays of the TMJ are usually negative in early stages but often show late-stage bone destruction, which may result in an anterior open-bite malocclusion. The diagnosis is suggested by TMJ inflammation associated with polyarthritis and is confirmed by other findings typical of the disease.
Treatment is similar to that of rheumatoid arthritis in other joints. In the acute stage, nonsteroidal anti-inflammatory (NSAID) drugs may be given, and jaw function should be restricted. An oral appliance worn during sleep is often helpful. When symptoms subside, mild jaw exercises help prevent excessive loss of mandibular motion. Surgery is necessary if ankylosis develops but should not be done until the condition is quiescent.
Condylar Hyperplasia
Slowly progressive unilateral enlargement of the head and neck of the condyle causes crossbite malocclusion, facial asymmetry, and shifting of the midpoint of the chin toward the unaffected side. The patient may appear prognathic. The lower border of the mandible is often convex on the affected side. Chondroma and osteochondroma may cause similar symptoms and signs, but they grow more rapidly and may cause even greater asymmetric condylar enlargement.
Condylar Hypoplasia
This condition usually results from trauma, infection, or irradiation occurring during the growth period but may be idiopathic. The deformity involves fullness of the face, deviation of the chin toward the affected side, an elongated mandible, and flatness of the face on the unaffected side. (The side on which the ramus is short causes muscles to appear fuller; the muscles on the unaffected side are stretched so that side appears flatter.) Mandibular deviation causes malocclusion.
Diagnosis is based on a history of progressive facial asymmetry during the growth period and x-ray evidence of condylar deformity and antegonial notching (a depression in the inferior border of the mandible just anterior to the angle of the mandible). There is frequently a causative history.
Treatment consists of surgical shortening of the unaffected side of the mandible or lengthening of the affected side. Presurgical orthodontic therapy helps optimize results.
Cyst and Tumours of TMJ
Temporomandibular joint cyst and tumors are very uncommon but show symptoms similar to intra-articular disorders that make up most of these disorders. The complaints are mostly pain, malocclusion and swelling. The most common TMJ-specific benign tumors are osteoma, synovial cyst, ganglion cyst etc. The treatment of these cyst and tumors may be conservative or radical surgery depending on nature of pathology.
Best Doctor for TMD Treatment

What types of doctors treat TMD?
A primary care provider, such as a family practitioner, dentist or ENT specialist, may first diagnose your TMJ. Your doctor may refer you to an oral and maxillofacial specialist for further treatment. You may also see a pain-management specialist if your TMJ pain is severe. Dr. Parit Ladani is an eminent Oral and Maxillofacial Surgeon with experience of more than 15 year in the field and he is well trained to treat any Temporomandibular Joint Problems. Nuface Cleft and Maxillofacial Surgery Clinic is well equipped to treat any Temporomandibular Joint Problems.
When should I seek treatment for TMJ disorder?
If you experience common TMD symptoms such as jaw pain, difficulty opening your mouth or clicking and popping of the jaw, schedule a visit with your Oral and Maxillofacial Surgeon right away. You should also schedule an appointment if you grind or clench your teeth, as this can lead to TMJ dysfunction.
What treatments are available for TMJ disorders?
- In some cases, the symptoms of TMJ disorders may go away without treatment. If your symptoms persist, your doctor may recommend a variety of treatment options, often more than one to be done at the same time.
- Treatments range from simple self-care practices and conservative treatments to injections and open joint surgery. Most experts agree that treatment should begin with conservative, nonsurgical therapies, with surgery left as the last resort. We’ll explore a variety of TMJ treatments in the sections below.
FACT FILE
- The initial diagnosis and treatment of facial pain and temporomandibular disorders (TMD) is becoming a routine part of practice for many general dentists. Some studies estimate the prevalence of clinically significant TMD to be as high as five percent of the general population with as many as two percent seeking some form of treatment for it (Dekanter 1992, Sep; Goulet 1995, Nov).
- Clinical experience and published literature suggests that conservative, non-surgical interventions, may account for as high as a 74 to 85 percent positive response rate in symptomatic TMD patients (Okeson 1986, Apr; Greene 1988, Sep).
- Likewise, other sources have even suggested that almost all patients with TMD will improve with time, regardless of the type of treatment they receive (Green 1982, Aug; Mejersjo 1983, Jun; Greene 1988, Sep; Nickerson 1989; Okeson 1989; McNeill 1993). Consequently, very few individuals with this disorder will ever require surgical intervention.

TMD Treatment

What are some examples of nonsurgical TMJ treatments?
Primary goals in treatment of TMD are to alleviate pain and to improve mandibular biomechanical function. The importance of initial conservative approaches in the management of TMD cannot be overstated for reasons that are not yet fully understood. These treatment modalities, when adhered to for two to three months (either alone or in combination), often provide the majority of patients with relief and/or resolution of signs and symptoms.
Contemporary conservative TMD management may include any or all of the following:
Home Treatments for TMD
There are things you can do on your own to help relieve TMD symptoms. Your doctor may suggest you try some of these remedies together.
- Take over-the-counter medications such as Nonsteroidal anti-inflammatory drugs (NSAIDs), to relieve muscle pain and swelling.
- Use moist heat or cold packs. Apply an ice pack to the side of your face and temple area for about 10 minutes. Do a few simple jaw stretches (if your dentist or physical therapist OKs them). When you’re done, hold a warm towel or washcloth to the side of your face for about 5 minutes. Perform this routine a few times each day.
- Eat soft foods. Add yogurt, mashed potatoes, cottage cheese, soup, scrambled eggs, fish, cooked fruits and vegetables, beans, and grains to your menu. Cut foods into small pieces so you chew less. Skip hard, crunchy foods, chewy foods, and thick or large bites that require you to open wide.
- Avoid extreme jaw movements. Keep yawning and chewing (especially gum or ice) to a minimum and don’t yell, sing, or do anything that forces you to open wide.
- Don't rest your chin on your hand. Don’t hold the phone between your shoulder and ear. Practice good posture to reduce neck and facial pain.
- Keep your teeth slightly apart as often as you can. This will relieve pressure on your jaw. Put your tongue between your teeth to control clenching or grinding during the day.
- Learn relaxation techniques to help loosen up your jaw. Ask your TMJ Specialist if you need physical therapy or massage. Consider stress reduction therapy as well as biofeedback.
Traditional Treatments
Talk to your TMJ Specialist about these tried-and-true treatments for TMD:
Medications
- Pain relievers and anti-inflammatories. If over-the-counter pain medications aren't enough to relieve TMJ pain, your TMJ Specialist may prescribe stronger pain relievers for a limited time.
- Antidepressants. These medications are used mostly for depression, but in low doses, they're sometimes used for pain relief, bruxism control and sleeplessness.
- Muscle relaxants. These types of drugs are sometimes used for a few days or weeks to help relieve pain caused by TMJ disorders created by muscle spasms.
A splint or night guard
- These plastic mouthpieces fit over your upper and lower teeth so they don’t touch. They lessen the effects of clenching or grinding and correct your bite by putting your teeth in a more correct position.
- What’s the difference between them? You wear night guards while you sleep. You use a splint all the time. Your Oral and Maxillofacial Surgeon will tell you which type you need.
Dental work
- Undergo corrective dental treatments. These treatments include replacing missing teeth or using crowns, bridges or braces to bring your bite into proper balance and alignment.
Counselling
- Education and counselling can help you understand the factors and behaviours that may aggravate your pain, so you can avoid them. Becoming more aware of tension-related habits — clenching your jaw, grinding your teeth, leaning on your chin, biting fingernails or chewing pencils — will help you reduce their frequency.
What are some other TMJ treatments?
If conservative treatments are unsuccessful, your healthcare provider may suggest one or more of the following:
- Transcutaneous electrical nerve stimulation (TENS). This therapy uses low-level electrical currents to provide pain relief by relaxing your jaw joint and facial muscles. It can be done at the dentist's office or at home.
- Ultrasound. Deep heat applied to the joint can relieve soreness or improve mobility.
- Trigger-point injections. Pain medication or anesthesia is injected into tender facial muscles called "trigger points" to give relief.
- Radio wave therapy. Radio waves stimulate the joint, which increases blood flow and eases pain.
- Low-level laser therapy. This lowers pain and inflammation and helps you move your neck more freely and open your mouth wider.
- Botulinum Toxin (Botox®). These injections help reduce muscle mass and inflammation.
Surgical Treatment for Temporomabdibular Joint

Who’s a good candidate for TMJ surgery?
TMJ surgery should only be considered after all other treatment options have been tried and severe pain remains. While TMJ surgery is the best option for many people, it’s important to weigh your options and make an informed decision.
Surgical intervention is appropriate only when:
- There is identifiable pathology amenable to surgical intervention.
- There is resultant loss of mechanical function
- There is pain related to joint pathology
- Any of the above has failed to respond to non-interventional treatment and there is, as a result, persistent loss of enjoyment of normal mandibular function which is negatively affecting the patient’s well-being in a persistent and unremitting manner.
- There has been a thorough explanation of the relative pros and cons of a specific intervention, a review of the potential benefits, risks and complications.
A surgical assessment (work-up) will include:
- A complete review of the nature of the TMD and all treatment attempts to date
- Radiographic assessment including any or all of the following: dental panoramic radiograph, CT scan, MRI, bone scan.
- A thorough medical assessment to include medical risk factors that may affect the surgical outcome.
The following TMJ Articular Disorders are manageable with surgical intervention:
- Internal Derangements (disc displacement disorders)
- Non-Inflammatory (non-infective degenerative disorders; post traumatic degeneration)
- Inflammatory Disease (osteomyelitis, synovitis, Lupus, psoriasis, Rheumatoid Arthritis)
- Neoplasia
- Ankylosis
Your doctor may advise against TMJ surgery if:
- Your TMJ symptoms aren’t that severe. For example, you may not need surgery if your jaw makes a clicking or popping sound when you open it, but there’s no pain associated with it.
- Your symptoms aren’t consistent. You may have severe, painful symptoms one day that vanish the next. This may be a result of certain repetitive motions or overuse — such as talking more than usual on a given day, chewing a lot of tough food, or constant gum chewing — that caused fatigue in your TMJ. In this case, your healthcare provider may recommend that you rest your jaw for a few hours or days.
- You can open and close your jaw all the way. Even if you have some pain or tenderness when you open and close your mouth, your doctor may not recommend surgery because of the risks involved. They may instead suggest medication, physical therapy, or lifestyle changes to reduce symptoms.
- It’s important to be evaluated by a oral and maxillofacial surgeon who’s trained in TMD. They will perform a thorough examination of your symptomatic history, clinical presentation, and radiological findings to determine if surgery will be beneficial for your symptoms. Surgery is considered a last resort if nonsurgical alternatives are unsuccessful.
Types of TMJ Surgery

Arthrocentesis
- When other methods don't help, your doctor might suggest procedures such as: Arthrocentesis. It’s often recommended when the jaw suddenly locks in the closed position. It can also help reduce inflammation in the TMJ.
- Arthrocentesis is a minimally invasive procedure that involves the insertion of small needles into the joint so that fluid can be irrigated through the joint to remove debris and inflammatory by-products and can help reduce pressure that causes the joint to be stiff or painful. Arthrocentesis will help mobilize an entrapped disc.
- This minor procedure is performed in the office, usually under local anesthesia.The recovery time is short, and the success rate is high.According to medical literature, arthrocentesis averages an 80 percent improvement in symptoms.
- Arthrocentesis is usually a first-line treatment because it’s less invasive and has a high success rate when compared to some of the other, more complicated procedures. Arthrocentesis is usually combined with Intra articular injections.

Injections
In some people, corticosteroid, hyaluronic acid, PRF injections into the joint may be helpful. Infrequently, injecting botulinum toxin type A (Botox, others) into the jaw muscles used for chewing may relieve pain associated with TMJ disorders.

Arthroscopy.
- Arthroscopic surgery is considered a minimally invasive diagnostic and therapeutic procedure however it is usually done in the hospital out-patient setting.
- Most arthroscopic procedures are used for diagnosis, lysis of adhesions and lavage of inflammatory mediators within the superior joint space.
- This procedure is performed under general anesthesia. Your surgeon makes a small incision in front of the ear and inserts a small, thin instrument that contains a lens and light. This instrument is hooked up to a video screen, which allows your surgeon to examine the TMJ and surrounding area.
Indications for arthroscopic surgery include:
- TMJ pain and/or dysfunction
- Hypomobility (unilateral or bilateral) associated with internal derangements characterized by both self reducing or non-self reducing disc displacement
- Synovitis; fibrous adhesions;
- Hypermobility
- Minor Osteoarthritis
TMJ arthroscopy is contraindicated in patients
- who have infection in the TM Joint and/or the overlying tissues
- In those with bony ankylosis.
Depending on the cause of your TMJ pain, it also allows your healthcare provider a lot of freedom to do complex procedures on the joint, such as:
- Inflamed or scar tissue removal
- Realign disc
- Joint reshaping
- Medication injection
- Treatment goals include a reduction in pain and improved bio-mechanical function, as well as the formulation of an accurate diagnosis.
- Because arthroscopic surgery is performed through tiny incisions, there is less scarring, a shorter recovery time, less discomfort, and fewer complications compared with open-joint surgery.
- In some cases, arthroscopic surgery can be as effective for treating various types of TMJ disorders as open-joint surgery but it has some limitations as well. While minimally invasive, there is the potential for complications from the procedure itself and while they are uncommon, informed consent is required.

Open-joint surgery.
- If your jaw pain does not resolve with more-conservative treatments and it appears to be caused by a structural problem in the joint, your doctor or dentist may suggest open-joint surgery (arthrotomy) to repair or replace the joint.
- If you undergo open-joint surgery, you'll be given general anesthesia. Unlike arthroscopy, open surgery is the traditional procedure in which a long incision is made to insert instruments.
Open-joint surgeries may be necessary if:
- The bony structures that make up the jaw joint are wearing away.
- There are tumors in or around TMJ.
- There is severe scarring or bone chips in the joint.
- TMJ Ankylosis
- Compared to arthrocentesis and arthroscopy, open-joint surgery results in a longer healing time plus has a greater chance of tissue scarring and nerve injury. Still, there are instances in which open-joint surgery is the best solution. Your healthcare provider can help you determine which approach is suitable for your unique needs.
- Open-joint surgery consists of opening an incision a few inches long over the joint so your healthcare provider can operate on the joint itself. By performing open-joint surgery, your surgeon will be able to remove bony growths or excess tissue. They are also able to repair or reposition the disc if it’s out of place or damaged. If your disc is beyond repair, a discectomy may be performed. Your surgeon may replace your disc completely with an artificial disc or your own tissue. When the bony structures of the joint are involved, the surgeon may remove some of the diseased bone of the jaw joint or the skull. In some severe condition, your surgeon may advise for Joint Replacement.
Following are common procedure performed with Open Joint Surgery

CONDYLOTOMY
- Condylotomy is an osteotomy (a controlled fracture) performed through the condylar neck/vertical mandibular ramus. It is indicated for internal derangement, specifically and most predictably in the management of recurrent self-reducing disc displacement. It may be used in non-self reducing disc displacement and has been reportedly helpful in recurrent dislocation.
- It is theorized that the osteotomy allows antero-medial repositioning of the condyle by virtue of contraction of the lateral pterygoid muscle, which, in turn, fosters a “new equilibrium” of the condyle-disc relationship.
- Additionally, it may produce “condylar sag” which increases the joint space, thereby allowing for passive repositioning of the disc. The principle goal of this procedure is to allow pain free and unrestricted mandibular range of motion.

ARTHROPLASTY
- Arthroplasty is an umbrella term that refers to a group of TMJ surgical procedures approached with an incision directly into the joint itself.
- They are indicated for those patients with progressively debilitating internal derangement refractory to the non-surgical and minimally invasive techniques described above.
- Other indications include severe degenerative joint disease, the treatment of various pathologic processes and ankylosis.
- The majority of arthroplasty procedures performed are aimed at the treatment of damaged, diseased or malpositioned discs.
- Specifically, disc plication is advocated for restoring the normal condyle-disc relationship when an otherwise healthy disc is displaced antero-medially. In these scenarios, the displaced disc is repositioned postero-laterally by a combination of retro-discal tissue reduction and re-attachement, often combined with an anterior band release. The disc is then sutured to the lateral TMJ capsule.
- When a disc is damaged beyond repair, disc removal also known as a discectomy/ menisectomy is indicated. When a discectomy is performed, decisions regarding management of the condylar hard tissues, as well as disc replacement must be made.
- With respect to the condition of the condyle, severe disc pathology is often associated with significant underlying hard tissue changes that must be addressed either through a partial (high condylar shave) or total (gap arthroplasty) condylectomy. This simultaneously serves to increase the joint space and remove the underlying osseous pathology.
- Regarding the re-establishment of a soft tissue interface between the glenoid fossa and the condyle; a number of surgical options exist. These include autogenous regional or free-tissue grafts (temporalis muscle, dermis, cartilage, or fat), or alloplastic materials. Each is intended to fill in the resultant dead space in order to prevent bone-to-bone contact, and minimize the potential for the development of TMJ ankylosis.

PROCEDURES FOR HYPERMOBILITY
Surgical procedures for the treatment of chronic or recurrent TMJ dislocation can be divided into two subgroups;
- Those that limit the range of condylar movement,
- Those that remove the blocking factor that prevents the condyle from returning to its normal position within the glenoid fossa upon mandibular closing.
EMINECTOMY
- The “eminectomy” was the first technique used to eliminate the blocking factor preventing the mandibular condyle from returning to its rest position within the glenoid fossa. This procedure is performed through a standard pre-auricular approach. Following exposure of the articular eminence, it is osteotomized and removed, leaving a flat smooth surface anterior to the glenoid fossa over which the mandibular condyle can slide without any interference.
SURGICAL PROCEDURES THAT LIMIT THE TRANSLATORY PATH OF THE MANDIBULAR CONDYLE
- The surgical displacement of a portion of the zygomatic arch inferiorly to block excessive translation of the tmj condyle.
- Capsular plication to tighten the tmj capsule and limit translatory movement of the mandibular condyle.
- Lateral pterygoid myotomies.
- Condylotomy.
- The injection of a sclerosing solution into the tmj ligaments in order to induce scar formation may limit the movement of the mandibular condyle.

TOTAL JOINT RECONSTRUCTION
- Total TMJ reconstruction is defined as the replacement of the articulating surfaces of both the glenoid fossa and mandibular condyle.
- While many autogenous and alloplastic options for total TMJ reconstruction are viable, we favor the use of an ultra-high molecular weight polyethylene fossa designed to function against a condylar component consisting of a highly polished Cobalt-chromium-molybdenum alloy with titanium alloy coating.
- Alloplastic TMJ reconstruction is a biomechanical as opposed to a biological solution to advanced anatomic TMJ pathology.
The indications for alloplastic TMJ reconstruction include:
- Ankylosed, degenerated or resorbed joints with severe anatomic abnormalities
- Failure of autogenous grafts in the multiply operated patient
- Severe inflammatory joint disease such as rheumatoid arthritis
- Failed previous alloplastic reconstruction
- Recurrent ankylosis associated with excessive heterotopic bone formation
- With respect to total TMJ reconstruction, success is measured in terms of restoration of TMJ function. In our experience, careful patient selection has resulted in a substantial improvement in quality of life for a majority of our patients.
- However, due to the complex nature of TMJ function, it is extremely difficult to reconstruct any joint back to its normal pre-morbid function. Pain relief gained is often a secondary benefit.
- It must be stressed that total TMJ reconstruction, with some specific exceptions such as in patients with severe rheumatoid TM Joint degeneration, is an end-stage procedure, and that the need for reconstruction indicates severe pathology not amenable to any other treatment modality.
What To Expect After TMJ Surgery?

Recovery from a TMJ surgery depends on the person and the type of surgery performed.
How long do I need to stay in hospital after TMJ Surgery?
- Most TMJ surgeries are outpatient procedures, so you can usually go home the same day. You’ll be monitored in the recovery room to make sure that your vitals are stable before your medical team allows you to leave.
- If you had general anesthesia, you’ll wake up in the recovery room. You’ll likely feel some pain in the jaw. Let your nurse know if you’re experiencing discomfort so they can give you pain medicine and help you feel comfortable.3
- If you’re staying in the hospital overnight, you’ll be taken to your hospital room. For a total joint replacement, you may be at the hospital for three to five days before you’re able to go home. Hospitals and surgery centers may differ on their discharge policies.
When can I go back to work after TMJ Surgery?
Your surgeon can give you information about when you can expect to go back to work after your procedure. For minor procedures, this might be the next day. Open-joint procedures, on the other hand, may require several weeks off, depending on your job and the type of surgery.
Wound Care
Depending on the procedure you had, you may have bandages to wear for several days afterward. Your stitches may dissolve on their own or they may need to be removed at a follow-up appointment. Your surgeon will let you know when you can remove the bandage and when you can clean the area with soap and water.
Cold and Heat application
With most TMJ surgeries, you’ll experience swelling, bruising, jaw pain, and tenderness. Apply ice packs to the face for no more than 20 minutes at a time for the first day after surgery. Keep your head elevated using two or three pillows when resting to help with swelling. After 48 hours, you can apply warm heat from a heating pad or a microwaved wet washcloth to help with any discomfort. Your jaw will probably be swollen for a week or more after surgery.
Pain Control
For discomfort, your healthcare provider may prescribe pain medication or suggest taking over-the-counter medicines. They may prescribe muscle relaxants if you’re experiencing any spasms.
Bite
You may notice a change in your bite or clicking in your jaw. Let your healthcare provider know if this doesn’t resolve on its own as your joint heals over the days and weeks after your procedure.
Physiotherapy and splint
Physical therapy or jaw exercises can help to restore your jaw’s function and range of motion. Your surgeon may suggest that you see a physical therapist to start jaw exercises in the first week after your surgery.
Wear a splint or other device on your jaw at all times until your doctor tells you it’s OK to remove it.
Diet
With all TMJ surgeries, you’ll need to eat a soft diet during the healing process. This may start with liquid-based foods, like smoothies and soups. After several days, you may be able to add soft foods like yogurt, applesauce, oatmeal, soup, mashed potatoes, and eggs. Avoid hard, chewy, and crunchy food.
Your healthcare provider will let you know when you can start adding other foods to your diet. For total joint replacement surgery, this process may take up to eight weeks.
It may be easier to eat small amounts every few hours rather than large amounts at mealtimes.
Follow up
Your healthcare provider will probably suggest you schedule a follow-up appointment about two to three weeks after surgery to make sure everything’s healing correctly and discuss how you’re feeling.
Recovery time for various TMJ Surgery
Your recovery will depend on the procedure that you had done.
TMJ Surgery Anticipated Recovery Time
Arthrocentesis, arthroscopy A few days to a week
Arthrotomy, arthroplasty Two weeks
Joint replacement Three to eight weeks
What are possible complications of TMJ surgery?
- Loss of jaw movement. Everyone has some decrease in jaw mobility after surgery, because the jaw heals with scar tissue, which is harder and tighter than normal tissue. But jaw exercises will help jaw movement.
- Injury of facial nerves, sometimes resulting in partial loss of facial muscle movement or loss of sensation.
- Damage to nearby tissue, such as the bottom of the skull, blood vessels, or anatomy related to your hearing
- Infections around the surgical site during or after surgery
- Frey syndrome, a rare complication of the parotid glands (near your TMJ) that causes abnormal face sweating
- Adverse reaction to the materials in an artificial disc. The risk of tissue rejection is higher if artificial materials, rather than your own tissue, are used.

Frequently Asked Questions
Please reach us at drparitladani@gmail.com if you cannot find an answer to your question.
TMJ pain can return even after you’ve had surgery. With arthrocentesis, only debris and excess swelling is removed. This means that debris can build up in the joint again, or inflammation can reoccur.
TMJ pain can also return if it’s been caused by a habit like clenching or grinding your teeth (bruxism) when you’re stressed or while you sleep.
If you have an underlying immune condition that causes tissues to become inflamed, such as rheumatoid arthritis, TMJ pain can come back if your immune system targets the joint tissue.
In some cases, yes, but it depends on the cause. For example, if you’ve had a TMJ flare-up due to a temporary period of stress, your symptoms will likely subside once the stress is no longer a factor. However, if your TMJ pain is due to jaw misalignment or the way your teeth fit together, you will likely have chronic problems that will only improve with treatment.
What happens if TMJ disorder is left untreated?
Left untreated, TMJ disorder can lead to significant health problems, including chronic pain and inflammation. It can also cause bite issues, tooth erosion and long-term conditions such as sleep apnea, insomnia, depression and anxiety.
With proper intervention, TMJ dysfunction can be successfully treated. The first step is seeing your healthcare provider for an evaluation. It’s best to treat the condition early on before symptoms worsen.
Some TMJ symptoms are caused by factors out of your control, such as the way your bite fits together. However, in some cases, you may be able to reduce the risk of TMJ dysfunction by:
Practicing good posture.
Wearing a night guard, especially if you clench or grind your teeth.
Wearing a mouthguard when playing contact sports.
Practicing relaxation and stress-reduction techniques.
TMJ Ankylosis
TMJ Ankylosis released in 16 years old Girl.
Temporo-mandibular Joint Ankylosis
Nuface Cleft and Maxillofacial Surgery Clinic
B-105/106, Dhanashree Height, Bldg No. 42, Azad Nagar 2, Veera Desai Rd, Andheri W, Mumbai. 400053

